New Mindbloom Research Shows Groundbreaking Outcomes for PTSD

Summary:
Mindbloom has conducted one of the largest studies of ketamine therapy for PTSD to date, revealing rapid, transformative outcomes that offer new hope to millions.
Highlights:
- Effectiveness: 79% of participants responded to treatment and 60% achieved remission upon program completion
- Tolerability: 96% reported no side effects
- Speed: 62% achieved at ≥10-pt reduction in PTSD symptoms after just two sessions
- Reduction in Suicidal Thoughts: 83% who reported suicidal thoughts at baseline saw improvement after two sessions, and 79% reported full resolution upon completion
These findings signal a paradigm shift in trauma care: fast relief, sustained recovery, and unprecedented accessibility through Mindbloom’s guided at-home model.
Study overview:
This landmark analysis builds on a growing body of Mindbloom-led research, including the largest and second largest peer-reviewed studies of ketamine therapy to date.
- Population: Adults representative of the typical treatment-seeking PTSD population, with a mean baseline PCL-5 score of 51.1, indicating moderate-to-severe symptom severity
- Primary Cohort: 374 patients who self-identified PTSD as their primary indication, had a baseline PCL-5 score of ≥33, had no prior ketamine therapy, completed all six sessions, and provided baseline and post–Session 6 PCL-5 assessments
- Protocol: Six guided ketamine sessions completed over four to six weeks, supported by structured preparation, integration, and continuous clinician monitoring
- Measurement: Symptom change was tracked using the PTSD Checklist for DSM-5 (PCL-5), the gold standard for assessing PTSD severity and response
Why is PTSD so hard to treat?
More than 13 million Americans live with post-traumatic stress disorder each year1. Despite its prevalence, most treatments remain slow, costly, inconsistent, and struggle to meet the scale of need. Untreated PTSD drives higher rates of depression, suicide, and lost productivity, costing the U.S. an estimated $232 billion annually2.
- SSRIs can take 8–12 weeks to work, may help only 30–60% of patients, and can cause side effects in up to 50%3, 4,5, 6
- Therapy can require months of sessions, may help only ~45%, and can see ~40% dropout rates3, 4
- IV Ketamine can cost $700 per session7 and can remain largely inaccessible outside major cities
- Spravato may yield only ~15% remission, with twice-weekly in-clinic dosing8
For many, that means months of waiting, incomplete recovery, or no meaningful relief at all. The field needs a fast, tolerable, and more accessible standard of care.
How effective is Mindbloom for PTSD?
The results of this analysis are unprecedented. Mindbloom’s guided, at-home protocol achieved outcomes rarely seen in mental health care, representing a fundamental shift in what recovery from trauma can look like.
- 80% reported significant reduction in symptoms upon completion (measured as a 10+ point reduction in PCL-5 scores from baseline)
- 44% average reduction in PTSD symptom severity
When compared to studies of other treatment types, Mindbloom’s symptom reduction is up to:
- 91% stronger than studies of therapy3
- 63% stronger than studies of antidepressants3,9
- 57% stronger than the leading study of Spravato8

How safe is Mindbloom ketamine therapy for PTSD?
Safety is the foundation of any mental health treatment, and Mindbloom’s outcomes set a new standard. Across hundreds of clients, guided at-home ketamine therapy proved not only highly effective, but was also remarkably well tolerated. Nearly all participants completed treatment without any side effects.
- 96% of clients reported no side effects
- Only 4% experienced side effects of any kind
When side effects did occur, they were generally mild and transient. In contrast up to 50% of patients report side effects when taking antidepressants6.
How quickly does relief occur?
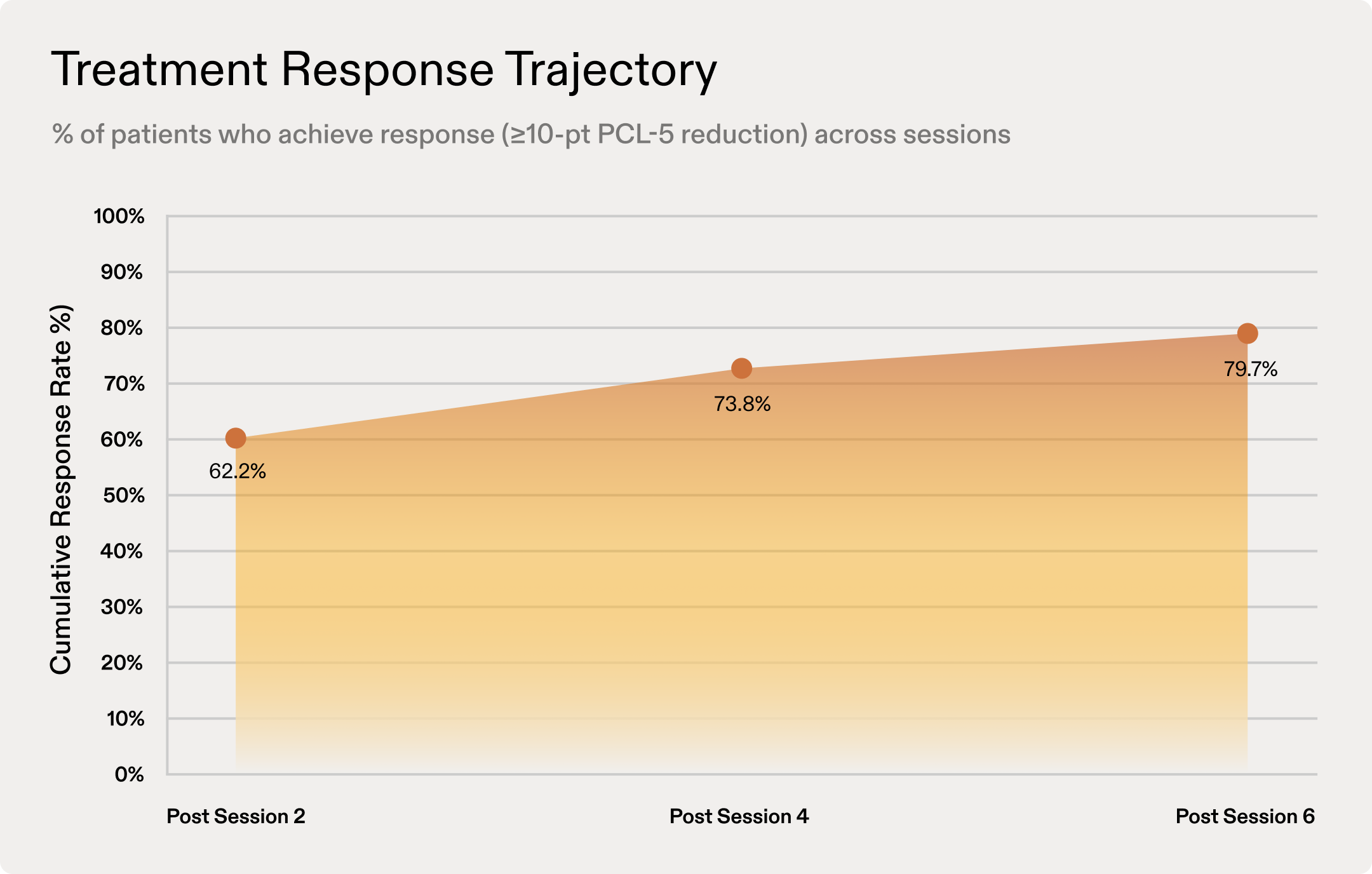
For many participants, healing began almost immediately. Within just two sessions, over half experienced signigicant improvements in PTSD symptoms, a pace rarely seen in psychiatric care. By the end of treatment, that population grew to nearly 8 in 10.
- 62% achieved meaningful improvement after just two sessions
- 80% responded by the end of six sessions
Does Mindbloom's protocol help with suicidal thoughts?
Suicidal ideation is one of the most urgent and dangerous symptoms of PTSD, yet traditional treatments often bring limited relief even after months of care. This study found that Mindbloom’s at-home protocol led to fast and substantial reductions in suicidal thoughts.
- 8 in 10 clients who began treatment with suicidal thoughts reported improvement after two sessions
- 3 in 4 experienced full resolution of those thoughts by program completion
The speed and magnitude of these results point to a critical advance in trauma care: the ability to deliver life-saving relief, outside of hospital clinic settings, and within days rather than months.
This study makes clear that the next chapter of trauma care has already begun. Healing that is fast, tolerable, and more accessible is no longer a promise, it’s happening now, and it’s changing lives. Read and download the full analysis here.
Want to learn more about at-home ketamine therapy?
- To learn more about Mindbloom’s at-home ketamine therapy, visit our homepage.
- If you’re ready to explore at-home ketamine therapy, take our brief candidate assessment.
- To better understand how ketamine interacts with your brain, read our guide on the neuroscience of ketamine.
- For safety information about ketamine, click here.
- Questions about Mindbloom? Reach out to our client relations team at support@mindbloom.com.
References:
- National Center for PTSD. (2024). How common is PTSD in adults? U.S. Department of Veterans Affairs. https://www.ptsd.va.gov/understand/common/common_adults.asp
- Davis, L. L., Umland, E., Ambrose, S., Kessler, R. C., & Le, T. (2022). The economic burden of posttraumatic stress disorder in the United States from a societal perspective. The Journal of Clinical Psychiatry, 83(6), 22m14592. https://www.psychiatrist.com/jcp/economic-burden-posttraumatic-stress-disorder-united-states-societal-perspective
- Rauch, S. A. M., Kim, H. M., Powell, C., Tuerk, P. W., Simon, N. M., Acierno, R., Allard, C. B., Norman, S. B., Venners, M. R., Rothbaum, B. O., Stein, M. B., Porter, K., Martis, B., King, A. P., Liberzon, I., Phan, K. L., & Hoge, C. W. (2019). Efficacy of prolonged exposure therapy, sertraline hydrochloride, and their combination among combat veterans with posttraumatic stress disorder: A randomized clinical trial. JAMA Psychiatry, 76(2), 117–126. https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2716980
- Fortney, J. C., Kaysen, D. L., Engel, C. C., Watkins, K. E., Hoge, C. W., Pietrzak, R. H., Rauch, S. A. M., et al. (2025). Pragmatic comparative effectiveness of primary care treatments for posttraumatic stress disorder: A randomized clinical trial.JAMA Psychiatry. Advance online publication. https://doi.org/10.1001/jamapsychiatry.2025.2962
- Montejo, A. L., Llorca, G., Izquierdo, J. A., Rico-Villademoros, F., & the Spanish Working Group for the Study of Psychotropic-Related Sexual Dysfunction. (2001). Incidence of sexual dysfunction associated with antidepressant agents: A prospective multicenter study of 1022 outpatients. Journal of Clinical Psychiatry, 62(Suppl 3), 10–21. https://www.psychiatrist.com/pdf/incidence-of-sexual-dysfunction-associated-with-antidepressant-agents-a-prospective-multicenter-study-of-1022-outpatients-pdf/
- Braund, T. A., Tillman, G., Palmer, D. M., Gordon, E., Rush, A. J., & Harris, A. W. F. (2021). Antidepressant side effects and their impact on treatment outcome in people with major depressive disorder: An iSPOT-D report. Translational Psychiatry, 11, Article 417. https://www.nature.com/articles/s41398-021-01533-1
- McInnes, L. A., Berman, R. M., Worley, M. J., & Shih, E. (2025). A retrospective analysis of ketamine intravenous therapy for post-traumatic stress disorder in real-world care settings. Psychiatry Research, 352, Article 116689. https://doi.org/10.1016/j.psychres.2025.116689
- Johnson & Johnson Innovative Medicine Medical Information. (2025, September 17). Use of SPRAVATO in patients with comorbid posttraumatic stress disorder (PTSD). Retrieved from https://www.jnjmedicalconnect.com/products/spravato/medical-content/use-of-spravato-in-patients-with-comorbid-posttraumatic-stress-disorder-ptsd
- Shiner, B., Westgate, C. L., Gui, J., Maguen, S., Young-Xu, Y., Schnurr, P. P., & Watts, B. V. (2018). A retrospective comparative effectiveness study of medications for posttraumatic stress disorder in routine practice. Journal of Clinical Psychiatry, 79(5), 18m12145. https://doi.org/10.4088/JCP.18m12145
This article is for informational purposes only and is not intended to be a substitute for professional medical advice. Always talk to your doctor about the risks and benefits of any treatment. If you are in a life-threatening situation, call the National Suicide Prevention Line at +1 (800) 273-8255, call 911, or go to the nearest emergency room.
More articles










